Master Your Costs: Co-Pays, Deductibles Explained!
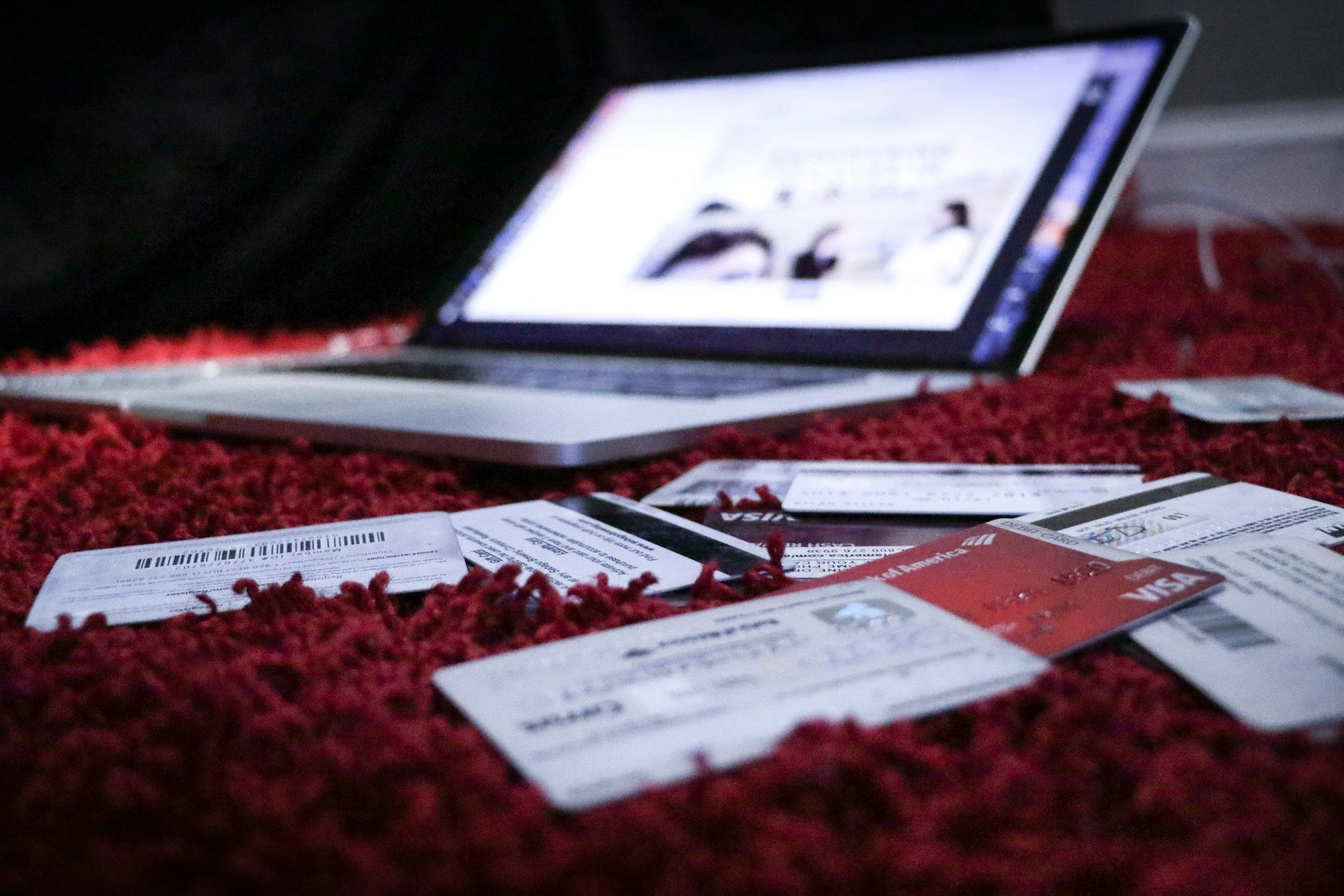
The Surprising Connection Between Financial Health and Physical Wellness
Have you ever felt a twinge of anxiety when the reception desk at your primary care clinic asks for your co-pay before you even meet the clinician? Or maybe you’ve walked out of your urgent care center and found yourself staring at a bill that doesn’t quite make sense. Why does health insurance have so many moving parts? How do co-pays, deductibles, and co-insurance really work? And why do clinicians insist on collecting these payments if you’re insured?
Believe it or not, the confusion surrounding these insurance mechanisms is extremely common—so common that research from the Kaiser Family Foundation indicates that a significant proportion of insured Americans misunderstand basic insurance terms. Beyond the practical implications for your wallet, misunderstanding your insurance coverage can also affect your physical wellness, leading some people to delay needed medical care or avoid it altogether due to cost concerns.
In this comprehensive blog post, we’re going to unravel the complexities of health insurance. Our focus is on three key components: co-pays, co-insurance, and deductibles. These terms might sound daunting, but once you understand how each one works—and why they exist in the first place—you’ll be better equipped to make informed decisions about your healthcare, whether you’re visiting a family practice, a primary care clinic, or an urgent care near you. By the end of this article, you’ll gain not only the definitions but also the deeper “why” behind insurance structures, the legal and ethical obligations your clinician faces when collecting your share of medical costs, and the potential ramifications if these obligations aren’t met.
But that’s not all. We’ll also provide practical tips and strategies to help you navigate your insurance benefits more effectively, reduce unnecessary out-of-pocket expenses, and ensure that your path to wellness remains both physically and financially viable. After all, wellness isn’t just about the absence of disease; it’s also about peace of mind. Let’s dive in.
Health Insurance Basics
The Role of Health Insurance in Modern Medicine
In today’s healthcare landscape, health insurance plays a pivotal role in allowing individuals and families to access medical services without bearing the full brunt of potentially exorbitant costs. If you’ve ever visited a primary care clinic or checked in for a procedure at an urgent care facility, you’ve likely encountered various fees that are partially offset by your insurance plan. The ultimate goal of insurance is to pool risk across many people. By paying a monthly premium, you join a group whose collective contributions help cover the medical expenses of any member who needs care.
However, understanding your insurance policy is crucial. If you’re confused about terms like “in-network” versus “out-of-network” or not sure why you need to pay a certain amount upfront, you’re not alone. Insurance can feel like a maze, but the first step is knowing the key terms and how they shape your healthcare experience.
Pro Tip: If you’re new to health insurance or you’ve changed jobs and have a new plan, take the time to carefully read your policy or summary of benefits. Contact your HR department or your insurance company’s customer service if you need clarification.
Overview of Insurance Terms You Should Know
Premium: The monthly fee you pay to your insurance carrier to maintain coverage. Think of this as your membership fee into the insurance pool.
Network: The group of healthcare providers (physicians, hospitals, labs, etc.) that have agreements with your insurance carrier. Staying “in-network” generally saves you money.
Claim: A formal request made by your healthcare provider to your insurance company for payment for services rendered.
Out-of-Pocket Maximum: The most you will pay for covered services in a given policy period (usually one calendar year). Once you reach this limit, insurance covers 100% of covered services.
These terms build the foundation for understanding the more specific elements we’ll explore next: co-pays, co-insurance, and deductibles.
Understanding Premiums, Networks, and More
It’s also important to recognize that your premium alone does not cover all your healthcare expenses. You might have the most comprehensive plan your employer offers, but you can still face costs when you visit a family practice doctor, primary care near you, or head to the urgent care near me. This is where co-pays, co-insurance, and deductibles come into play. They’re additional cost-sharing mechanisms designed to keep everyone—both patients and insurance companies—responsible for managing healthcare costs.
Want to understand more about how your insurance might affect the care you receive? Check out our Insurance and Payment Information Page on Innovative Urgent Care and Family Clinic to learn about accepted carriers and our financial policies.
What Are Co-Pays, Co-Insurance, and Deductibles?
In this section, we’ll define each of these cost-sharing mechanisms. Remember, while the vocabulary might seem complicated, each term simply describes a different way of splitting healthcare expenses between you and your insurance company.
Defining Co-Pays
A co-pay (short for co-payment) is a fixed amount you pay for a covered health service after you’ve paid your deductible (in plans that require a deductible for certain services) or even before meeting your deductible in some insurance plans. Typical co-pays might be $20 for a doctor’s visit, $10 for a generic prescription, or $40 for a specialist visit.
Example: Let’s say you visit your primary care clinic for a routine check-up. Your plan states you owe a $25 co-pay for each primary care visit. You pay $25 at the time of the visit, and your insurance covers the rest.
Defining Co-Insurance
Co-insurance is a percentage of the cost of a covered health service that you pay after meeting your deductible. A common co-insurance split might be 80/20, meaning the insurance pays 80% while you pay 20% of the allowable charges.
Example: Suppose you’ve already met your deductible, and you receive a bill for a covered surgery amounting to $10,000. With an 80/20 co-insurance plan, your insurance would cover $8,000, and you would be responsible for $2,000.
Defining Deductibles
A deductible is the amount you must pay out of pocket for certain covered healthcare services before your insurance plan starts sharing those costs. Deductibles can vary widely. Some people have a $500 annual deductible, while others might have $5,000 or more.
Example: Let’s say your insurance plan has a $1,000 deductible. If you require a medical procedure costing $2,500, you’d pay the first $1,000, and then your insurance would start to cover costs according to your co-insurance rate for the remaining $1,500.
How These Costs Work Together
To illustrate how these three elements can interact:
First, you pay your deductible for applicable services.
Next, you owe co-insurance on any remaining costs after your deductible has been met.
Throughout this process, you might also have co-pays for specific services like office visits or prescriptions.
This layered approach to cost-sharing is how your plan ensures that both you and the insurance company are contributing to your healthcare expenses. Understanding these steps helps you budget for your medical expenses and avoid surprises.
Why Do These Costs Exist?
Risk-Sharing and Cost Control
Insurance companies use co-pays, co-insurance, and deductibles to make sure that the financial risk is spread out. In simpler terms, rather than having the insurance company pay for 100% of every claim (which would result in extremely high premiums for everyone), these mechanisms ensure that patients have some skin in the game. This shared responsibility also helps prevent overuse of healthcare services—if something is entirely free, people may utilize it more often than necessary, driving up overall costs.
From a clinician’s perspective, these insurance structures can also help maintain a steady flow of income. With certain payments due upfront, healthcare providers have some financial stability even before the insurance claim is processed. This balance is crucial for maintaining the sustainability and quality of services in a primary care clinic, family practice, or urgent care near me.
Encouraging Responsible Healthcare Choices
When you have to pay a co-pay or meet a deductible, you’re more likely to weigh the necessity of each medical service. While this can be a double-edged sword—sometimes people forego essential care due to cost—it can also prevent unnecessary emergency room visits or expensive tests that might not be clinically justified. Ideally, this cost-sharing encourages individuals to explore wellness options, preventive services, and more cost-effective providers.
The Role of Insurance Companies and Healthcare Providers
Insurance companies negotiate contracts with healthcare providers to determine how much will be paid for each service. These contracts are why you see a difference between “in-network” and “out-of-network” providers. In-network providers agree to negotiated rates, ensuring you pay less out of pocket. In turn, these providers expect payment from both the insurance company and you (through co-pays, deductibles, or co-insurance).
For more insights on how our clinic operates within insurance networks, visit our Services Page to learn about the range of care options available at Innovative Urgent Care and Family Clinic.
Why Are Clinicians Required to Collect Them?
Contractual Obligations with Insurance Carriers
One of the most common misconceptions among patients is that their clinicians can waive co-pays or avoid collecting deductibles. In reality, when a primary care clinic or urgent care center signs a contract with an insurance carrier, they agree to certain terms. One of those terms is that they must collect co-pays and deductibles as outlined in the insurance policy.
Failure to collect these payments can be considered a breach of contract, as it undermines the entire cost-sharing structure. Insurance carriers base their premium and payout calculations on the assumption that patients will pay their share of the costs. If a clinician continually waives co-pays or deductibles, the insurance company may terminate the contract or take legal action.
Legal and Ethical Considerations
Beyond contractual obligations, there are also legal considerations. In some jurisdictions, waiving co-pays or deductibles for patients with insurance can be construed as fraud, particularly if the clinician bills the insurance for a higher amount. This is because the insurer is not receiving accurate information about the true cost of services and the contributions made by the patient.
Moreover, from an ethical standpoint, clinicians generally aim to uphold equity in healthcare. If co-pays and deductibles are waived for some patients arbitrarily, it can create an unfair system. While clinicians often show compassion for patients in financial distress, there are specific guidelines they must follow to offer any form of financial relief.
Ensuring the Sustainability of Healthcare Practices
Collecting co-pays and deductibles isn’t just about following the rules—it’s also about ensuring that healthcare practices remain financially viable. Running a primary care clinic or family practice is costly. There are overhead expenses, salaries, medical equipment costs, rent, and supplies. Collecting these patient obligations helps keep the doors open so that clinicians can continue to offer quality care to the community.
Pro Tip: If you are struggling to pay your co-pay or deductible, talk to your healthcare provider about possible payment plans or financial assistance options. Communication is key, and many providers want to work with patients to ensure they receive necessary care without undue financial strain.
Ramifications for Not Paying Your Share
Potential Violations of Insurance Contracts
If a clinician does not collect or a patient does not pay the required co-pay, co-insurance, or deductible, it can be seen as a violation of the contract between the healthcare provider and the insurance company. From the insurance company’s standpoint, this is a form of cost-shifting, where they’re effectively paying more than their share based on the policy design. This can lead to:
Audits: Insurance companies often audit providers to ensure compliance.
Fines or Penalties: If found in violation, a provider could face fines.
Loss of Network Participation: Repeated violations can result in a provider being removed from the insurance network, limiting their ability to serve insured patients.
Impacts on Future Care and Insurance Policies
For patients, repeatedly not paying co-pays or deductibles can have personal ramifications:
Collection Notices: Unpaid medical bills can be sent to collections, harming your credit score.
Denied Claims: Insurance companies may deny future claims if they suspect cost-sharing obligations are not being met.
Policy Changes or Premium Increases: If insurers see high levels of non-payment, they might raise premiums or adjust policies to compensate for perceived risk.
The Trickledown Effect on Overall Healthcare Costs
At a systemic level, widespread non-payment of co-pays and deductibles can drive up healthcare costs for everyone. If insurance companies are consistently reimbursing healthcare providers more than planned, they may raise premiums to offset these losses. This results in higher monthly payments for policyholders—yet another reason why it’s crucial for everyone to pay their share.
For a more detailed discussion about insurance obligations and legal considerations, you can consult the American Medical Association (AMA) website, which frequently publishes resources on ethical and legal standards in healthcare billing.
In-Depth Expert Insights
The Healthcare Provider’s Perspective
From the vantage point of a clinician, particularly in a primary care clinic or family practice, it’s important to remember that every patient interaction combines medical expertise with financial considerations. While clinicians are primarily focused on providing the best possible care, they also have to navigate insurance rules, billing processes, and contractual obligations.
Balancing Care and Cost
Healthcare providers often find themselves walking a fine line: wanting to offer compassionate, patient-centered care on one hand, and needing to collect payments as required by law and contract on the other. This can be especially challenging in communities where many patients are under-insured or struggle financially. Nonetheless, adhering to cost-sharing requirements is critical for maintaining trust with insurance carriers and ensuring the longevity of the practice.
Patient Case Studies: Common Pitfalls and Success Stories
Let’s examine two hypothetical scenarios that highlight how patients can navigate these financial waters.
Sarah’s Surprise Bill
Situation: Sarah, a 29-year-old teacher, visits an urgent care near her for a sprained ankle. She pays her $50 co-pay, assuming that’s all she’ll owe. Weeks later, she receives a bill for $200 because she hadn’t met her deductible, and her co-insurance also applied.
Pitfall: Not realizing that co-pays might not cover the full cost if a deductible or co-insurance is still in effect.
Solution: By reviewing her insurance summary of benefits beforehand, Sarah could have anticipated additional charges. Now, she speaks with the billing department and arranges a payment plan that fits her budget.
Carlos’s Preventive Care Advantage
Situation: Carlos, a 45-year-old warehouse manager, schedules an annual check-up at a family practice for routine bloodwork and immunizations. He learns that preventive services are fully covered, so he has no co-pay or deductible costs for that particular visit.
Success: Carlos maximizes his insurance benefits by understanding that many preventive services—like annual check-ups, routine immunizations, and screening tests—come at no out-of-pocket cost under the Affordable Care Act guidelines (for in-network providers).
Lesson: Knowledge is power. By proactively researching his plan, Carlos saves money and stays on top of his health.
These scenarios underscore the importance of reading your policy details and staying in communication with both your insurer and your healthcare provider.
Trends in Health Insurance Policies: What’s Changing?
Insurance policies evolve based on legislation, market trends, and consumer needs. Recent trends include:
High-Deductible Health Plans (HDHPs): These plans feature lower premiums but higher deductibles, making them attractive to people who rarely use healthcare services. However, they do pose higher out-of-pocket costs if you get sick or injured.
Value-Based Care Models: Some insurance carriers are shifting toward reimbursing providers based on health outcomes rather than fee-for-service models. This can affect how co-pays and deductibles are applied, especially for chronic disease management.
Telemedicine Coverage: Many insurance plans now include virtual visits, sometimes at reduced or no co-pay rates, especially for mental health services.
Interested in how telemedicine works within our practice? Check out our Telemedicine Services at Innovative Urgent Care and Family Clinic to see if it’s an option for your next visit.
Navigating Your Insurance
The reality is that insurance can be confusing. But with the right information and tools, you can minimize surprises and maximize the value of your coverage.
Verifying Your Coverage: A Step-by-Step Guide
Check Your Insurance Card: Identify your plan type and member ID.
Visit Your Insurer’s Website: Create an online account to review your plan documents, in-network providers, and remaining deductible or out-of-pocket balance.
Call Customer Service: If something is unclear, ask directly about co-pay amounts, co-insurance percentages, and whether you’ve met your deductible.
Confirm With Your Provider: Before scheduling a procedure or visit, contact your primary care clinic to confirm they are in-network and understand any expected costs.
Talking to Your Provider About Costs
Communication is crucial. When you call to make an appointment or arrive for your visit:
Ask for an Estimate: While it’s not always possible to get an exact amount, a ballpark figure can help you plan.
Discuss Payment Plans: If you anticipate a large bill, ask about installment plans. Many clinics offer them.
Inquire About Discounts: Some providers have special rates for cash-paying patients or discounts for financial hardship cases.
Maximizing Benefits and Minimizing Out-of-Pocket Expenses
Use Preventive Services: Take advantage of fully covered annual physicals, immunizations, and screenings.
Stay In-Network: Whenever possible, see providers and use facilities that your insurance classifies as “in-network.”
Track Your Deductible: If you’re close to meeting your deductible, consider scheduling procedures to take advantage of your co-insurance coverage once the deductible is met.
Consider an HSA or FSA: Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) can lower your taxable income while setting aside money specifically for healthcare expenses.
Coping Strategies if You’re Under-Insured or Uninsured
If you’re in a situation where you have minimal or no insurance coverage:
Explore Community Resources: Free or low-cost clinics may be available for basic medical needs.
Shop Around: Comparing costs for procedures or imaging at different facilities can significantly reduce your expenses.
Seek Negotiated Cash Rates: Many providers offer discounted rates for patients who pay in cash at the time of service.
The National Association of Free and Charitable Clinics offers a database of charitable clinics that provide healthcare for the uninsured or under-insured.
Insurance in the Context of Wellness
How Financial Health Affects Physical Health
It might surprise some to learn how intertwined financial stress is with physical health. Chronic stress over medical bills can contribute to mental health issues such as anxiety and depression, which, in turn, can worsen physical conditions like hypertension or diabetes. Conversely, having a solid understanding of your insurance plan can reduce stress and encourage you to seek timely care at an urgent care near me or a family practice for preventive check-ups and treatments.
Integrating Preventive Care and Wellness Strategies
Preventive care services often come with lower or no out-of-pocket costs, especially if you stay in-network. Many insurance plans encourage annual check-ups, routine blood tests, and screenings for common conditions like hypertension, diabetes, and certain cancers. Taking advantage of these benefits not only saves money but also supports your long-term wellness goals.
At Innovative Urgent Care and Family Clinic, we emphasize a holistic approach to health, which includes:
Weight Loss Management: Excess weight is linked to numerous health issues, from cardiovascular disease to joint problems. By working with a specialist, you can create a sustainable plan to achieve a healthier weight.
Hormone Replacement Therapy (HRT): For patients experiencing hormonal imbalances—whether due to menopause, thyroid issues, or other conditions—HRT can be a game-changer. It’s essential to confirm your insurance coverage for such treatments to understand any associated co-pays, co-insurance, or deductibles.
For more details on our approach to wellness and how insurance may apply, visit our dedicated pages on Weight Loss Management and Hormone Replacement Therapy at Innovative Urgent Care and Family Clinic.
Aligning Insurance with Weight Loss Management and Hormone Replacement Therapy
While some insurers cover weight loss counseling or hormone therapy if it’s deemed medically necessary, others may categorize these services as elective or partially covered. Always verify coverage before initiating a new treatment plan. Ask questions like:
Is the service coded as preventive, diagnostic, or treatment-based?
Do I need pre-authorization for coverage?
What is my specialist co-pay or co-insurance rate for these services?
Knowing these details can help you budget and plan for your treatments more effectively.
Harnessing Knowledge for Better Health
The labyrinth of co-pays, co-insurance, and deductibles might seem daunting at first, but they serve a critical function in our healthcare system: cost-sharing, risk management, and ensuring that healthcare practices remain viable. As a patient, understanding these terms not only empowers you to make informed decisions but also helps you manage your financial stress, enabling you to focus on what truly matters—your health and wellness.
By knowing why co-pays, co-insurance, and deductibles exist, and understanding that clinicians who are contracted with insurance carriers must collect them to stay compliant and financially stable, you equip yourself with the knowledge to navigate our healthcare system more confidently. You also become an active participant in maintaining the integrity of this system, preventing unpaid balances from spiraling into bigger issues like increased premiums, collections, or loss of in-network coverage.
Key Takeaways
Co-Pays: Fixed amounts paid for specific services, such as doctor’s visits or prescriptions.
Co-Insurance: A percentage-based payment model that kicks in after you meet your deductible.
Deductibles: The amount you must pay before your insurance covers certain services.
Why They Exist: They distribute costs between you and your insurance carrier, helping control healthcare usage and maintain financial viability for clinics.
Why Clinicians Must Collect Them: Contractual obligations, legal considerations, and ethical practice standards mandate that healthcare providers enforce co-pays and deductibles.
Ramifications of Non-Payment: Violating insurance contracts can lead to audits, fines, and higher premiums for everyone. Patients may face collections, damage to credit, and potential denial of future claims.
Navigating the System: Verify your coverage, communicate with providers, use preventive services, and consider an HSA or FSA if available.
Wellness Matters: Insurance is a tool that supports comprehensive care, including weight loss management and hormone replacement therapy, so you can optimize your health at every stage of life.
Remember, an ounce of prevention is worth a pound of cure—not just clinically but also financially. So take control by becoming informed, staying proactive, and never hesitating to ask questions. By doing so, you’ll ensure that your journey toward better health is as smooth and cost-effective as possible.
Explore more on our Wellness Programs at Innovative Urgent Care and Family Clinic to see how we integrate preventive care with insurance-friendly solutions.
Learn more about various plan structures and regulations at HealthCare.gov.
Thank you for reading this comprehensive guide. We hope it helps you feel more confident about navigating co-pays, co-insurance, and deductibles. Your health is an investment—both physically and financially—so make sure you’re making the most of your coverage. If you have any questions or would like to schedule an appointment, please don’t hesitate to contact us at Innovative Urgent Care and Family Clinic. We’re here to support you on your path to wellness.